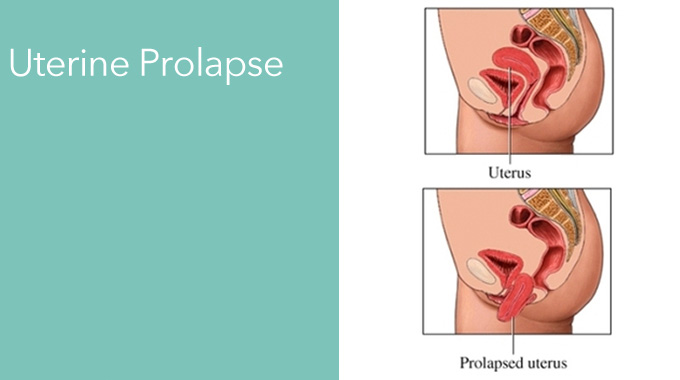
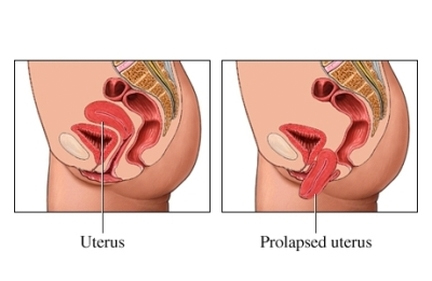
Prolapse Definition
Uterine prolapse (“dropped uterus”) is a condition in which a woman’s uterus (womb) sags or slips out of its normal position. The uterus may slip enough that it drops partially into the vagina (the birth canal), creating a perceptible lump or bulge. This is called incomplete prolapse. In a more severe case—known as complete prolapse—the uterus slips to such a degree that some of the tissue drops outside of the vagina.
Women with mild cases of uterine prolapse may have no obvious symptoms. However, as the slipped uterus falls further out of position, it can place pressure on other pelvic organs—such as the bladder or bowel—causing a variety of symptoms, including:
- Pelvic pressure: a feeling of heaviness or pressure in the pelvis
- Pelvic pain: discomfort in the pelvis, abdomen or lower back
- Pain during intercourse
- A protrusion of tissue from the opening of the vagina
- Recurrent bladder infections
- Unusual or excessive discharge from the vagina
- Constipation
- Difficulty with urination, including involuntary loss of urine (female incontinence), or urinary frequency or urgency 1
Symptoms may be worsened by prolonged standing or walking, due to added pressure placed on the pelvic muscles by gravity.
Causes of Uterine Prolapse
Trauma incurred during the birthing process, particularly with large babies or after a difficult labor and delivery, is one of the main causes of the muscle weakness that leads to uterine prolapse. Reduced muscle tone from aging, as well as lowered amounts of circulating estrogen after menopause, may also form contributing factors in pelvic organ prolapses. In other circumstances, uterine prolapse may be caused by fibroids or other tumor in the pelvic cavity. Genetics also may play a role; women of Northern European descent experience a higher incidence of uterine prolapse than do women of Asian and African heritage. Finally, increased intra-abdominal pressure, stemming from such diverse conditions as obesity, chronic lung disease and asthma, can be contributing factors in uterine prolapse.
Stages of Uterine Prolapse
Four stages of uterine prolapse are commonly defined:
- Stage I of uterine prolapse is defined as descent of the uterus to any point in the vagina above the hymen (or hymenal remnants).
- Stage II of uterine prolapse is defined as descent to the hymen.
- Stage III of uterine prolapse is defined as descent beyond the hymen.
- Stage IV of uterine prolapse is defined as total eversion or procidentia.6
Uterine prolapse always is accompanied by some degree of vaginal vault prolapse.
Treatment
How is uterine prolapse treated?
There are surgical and non-surgical options for treating uterine prolapse. The treatment chosen will depend on the severity of the condition, as well as the woman’s general health, age and desire to have children. Treatment generally is effective for most women. Treatment options include the following:
Non-surgical Options
Exercise – Special exercises, called Kegel exercises, can help strengthen the pelvic floor muscles. This may be the only treatment needed in mild cases of uterine prolapse. To do Kegel exercises, tighten your pelvic muscles as if you are trying to hold back urine. Hold the muscles tight for a few seconds and then release. Repeat 10 times. You may do these exercises anywhere and at any time (up to four times a day).
Vaginal pessary – A pessary is a rubber or plastic doughnut-shaped device that fits around or under the lower part of the uterus (cervix), helping to prop up the uterus and hold it in place. A health care provider will fit and insert the pessary, which must be cleaned frequently and removed before sex.
Estrogen replacement therapy (ERT) – Taking estrogen may help to limit further weakness of the muscles and other connective tissues that support the uterus. However, there are some drawbacks to taking estrogen, such as an increased risk of blood clots, gallbladder disease and breast cancer. The decision to use ERT must be made with your doctor after carefully weighing all of the risks and benefits.
Surgical Options
Hysterectomy – Uterine prolapse may be treated by removing the uterus in a surgical procedure called hysterectomy. This may be performed with a mimimally invasive technique using the da Vinci Robotic or by vaginal, laparoscopic or abdominal hysterectomy. Hysterectomy is major surgery, and removing the uterus means pregnancy is no longer possible.
Uterine or vaginal suspension – This procedure involves putting the uterus, cervix or vagina back into its normal position. This may be done by reattaching the pelvic ligaments to the lower part of the uterus or vagina to hold it in place. Another technique uses a special mesh material that acts like a sling to support the cervix or vagina in its proper position. Recent advances include performing this with minimally invasive robotic techniques (through small band aid sized incisions) that decrease post operative pain and speed recovery.
Losing weight, stopping smoking and getting proper treatment for contributing medical problems, such as lung disease, may slow the progression of uterine prolapse. However, without treatment, you may continue to lose uterine support, which could require future treatment.